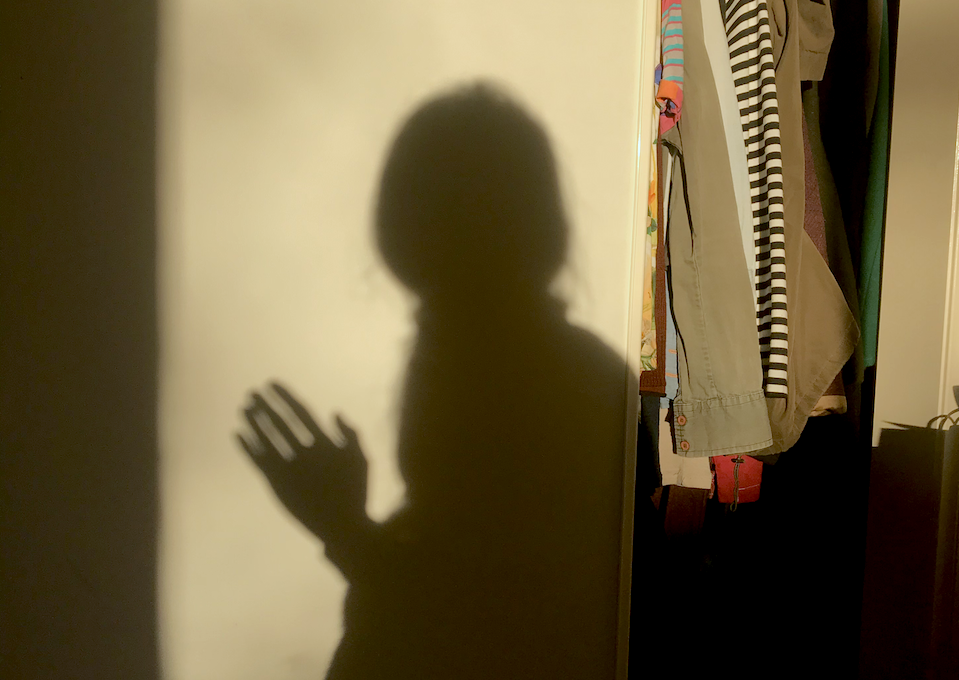
For chronically ill and disabled people, invisibility is a web we are constantly tangled in.
Invisibility is all too common in social interactions, social expectations, structural inaccessibility, or through bias in the medical system. Most of us have experienced at least one of these scenarios, and depending on the disability or intersectionality, it can mean ticking all of the above.
The terms “invisible illness” and “hidden disability” are used interchangeably to describe a myriad of illnesses, conditions and disabilities which may not be immediately apparent. There is incredible advocacy in this space (such as the Hidden Disabilities Sunflower Lanyard) which seeks to raise awareness and point to an individual’s support needs when they may otherwise be overlooked.
I recently experienced the positive impact of this advocacy when wearing the Hidden Disabilities Sunflower Lanyard while travelling. This internationally recognised symbol for invisible and hidden disabilities enabled me to get some additional support in the airports, which was a gamechanger for making the trip more accessible to me.
And yet, while the terms “invisible” illness and “hidden” disabilities have been globally adopted; I have found myself questioning, are we pigeonholing ourselves into labels that may not always be in our best interests?
Invisibility is about the observer’s perception
In my experience, the idea that a condition is “invisible”, most of the time is not actually true. I live with multiple chronic illnesses including POTS (Postural Orthostatic Tachycardia Syndrome), MCAS (Mast Cell Activation Syndrome), small fibre neuropathy, and hypermobility, and the following are just some examples of outwardly visible or tangible indicators of my conditions:
- Cold hands
- Yawning, and being short of breath
- Excessive blinking
- Memory loss or difficulty in word finding
- Losing my train of thought mid-sentence
- Slow movement
- No appetite
- Being scattered, distracted, unresponsive, indecisive
- Fidgeting
- Leaning on everything, or holding my head in my hands when seated at a table
- Sitting in unusual positions, pulling my leg up or twisting my legs (pretzel legs)
Suffice to say, most of this list is often swept under the rug as fairly common human experiences. Many in the chronic illness and disability community have the shared experience of being perceived as “well”, but the reality is: you often can’t tell how someone is feeling by looking at them. Invisibility says more about the perception of the observer than it does the affected person. And this concerning issue seeps into the medical system.
There is a long history of illness and disabilities being undiagnosed, mislabeled and dismissed. Medical gaslighting and disbelief of patients is rampant and continues to delay diagnoses for many for years – and even decades. Neither “invisible” or “hidden” are medical terms, and yet symptom or disability presentation is often equated with doubt or cynicism about the truth of an illness or disability. This is often used to reinforce the narrative that a patient’s support and medical care needs aren’t valid, that we are exaggerating or even making it up entirely, and asks us to repeatedly prove we are sick enough to get help. However, there is a very fine line between fighting to be seen, and hiding symptoms in order to “get on with life”.
“Hidden disabilities”
Hiding symptoms or a disability is all too real for many chronically ill and disabled people, as we try to warp ourselves to fit into a world that’s not designed to support us. Some of us have spent our whole lives attempting to contort our bodies and suppress symptoms to get through the day due to delayed or misdiagnoses. In this context, masking is the result of not feeling safe to be seen as we are and is a protective mechanism. And yet, the masking of symptoms is exhausting and can lead to exacerbated symptom severity or permanent harm.
I have only recently started identifying as disabled, because due to delayed diagnoses, misdiagnoses and medical gaslighting I share the common experience for those with dynamic conditions whereby I push past my limits by masking symptoms.
Where Crip Theory aims to challenge the notion that certain bodies and abilities are the “default” or “normal”, here we can draw on this idea to normalise invisible illness and hidden disabilities as valid and thus reduce the toll of masking.
What terms can we use instead?
I’m not going to lie, I am one of many people who use the terms “invisible” and “hidden”, and find both comfort and community under these identifiers. My critique of these terms is not intended to undermine their usefulness and place in community and advocacy work, as these banners can be really helpful for drawing attention to our experiences. Instead, I am questioning what we are identifying with and if it is necessary in all contexts.
If using these identifiers aligns with you, do keep using them, I know I will be. But let’s think about it differently for a moment. Are these labels part of what is binding us to the cycle of masking, gaslighting and medical dismissal? Does this language encourage complacency in the face of visible symptoms within medical or social environments?
A part of the aim of disability advocacy is to challenge societal norms. I want to ensure the way we are perceived, heard and seen does not affirm or reinforce ableism by making visibility the responsibility of the ill or disabled person.
Language is powerful, and it may not always be of benefit to use these terms unless we are also pointing to what is visible. And while it may be ambitious, who knows, this could even lead to removal of social and structural barriers, access to adequate support, reducing diagnostic delays, and disability pride.
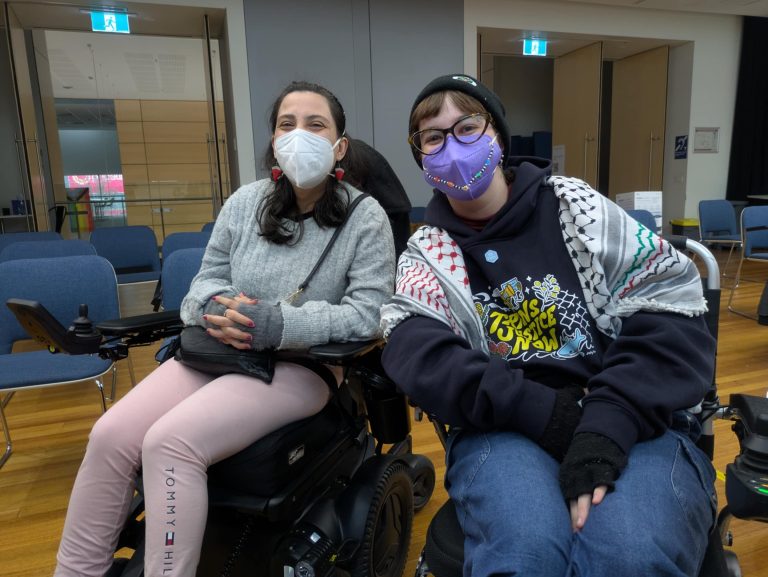
Autumn Tansey is a Naarm (Melbourne) based visual artist and curator with a concept-led practice. Working across photography, video, projection, installation and sculpture; Autumn creates dynamic imagery and installations responding to site, materiality, and politics informed by life with chronic illness and disabilities and the climate crisis. Autumn has also managed and curated arts projects in the public and private sector, with a particular interest in creating works in the public realm.
Since completing a Bachelor of Fine Arts (Photomedia) in 2010, Autumn has been the recipient of various awards, residencies and commissions including; National Gallery of Victoria’s ‘NGV Studios’ Residency, Kayell Australia Excellence in Photo-Media Award, and the Alliance Française Prize for Monash University Graduates. Recent highlights include being a Wyndham Art Prize 2026 Finalist, Incinerator Art Awards 2024 Finalist, and Grieve Project Awards 2024 Longlisted.
@autumntansey
www.autumntansey.com
Want to write for the Belong Blog? Pitch us your ideas. Our blog is open to all people in Australia who identify as having a disability. Contact Zoe@drc.org.au for more.
Looking for a disability-led, radically accessible group where you can be yourself, connect, and feel supported? Join Belong today.